A Lower Segment Caesarean Section (LSCS) is the most frequently used type of Caesarean section during childbirth. This surgical procedure involves making a transverse incision approximately 1-2 centimeters above the attachment point of the urinary bladder to the uterus, referred to as the Pfannenstiel incision.
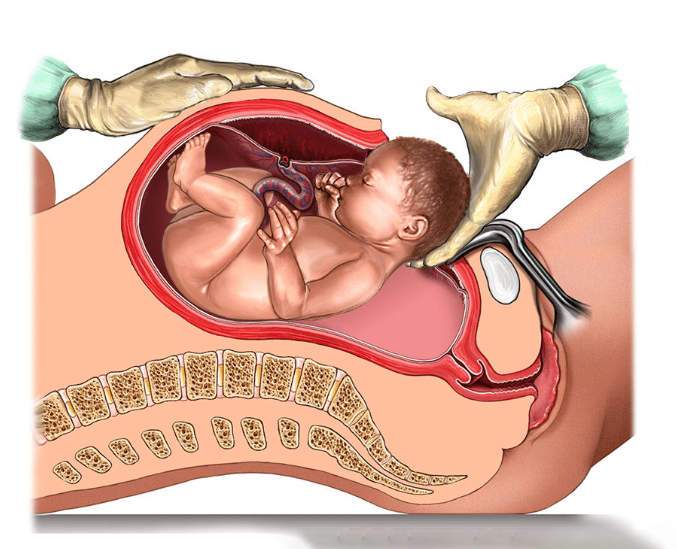
This location is known as the lower segment of the uterus. The lower segment incision has certain advantages, such as reduced blood loss and easier repair than other Caesarean sections.
LSCS Incision Types
The incision in an LSCS may be transverse, which is the typical approach, or vertical in specific situations:
- Presence of lateral varicosities
- A constriction ring that needs to be cut through
- Deeply engaged fetal head
The choice between transverse and vertical incisions depends on the clinical conditions.
Advantages Of The Lower Segment Location
The location of the incision in LSCS offers several advantages:
- The peritoneum is less tightly attached to the uterus, making the surgical procedure more efficient.
- Contractions are less pronounced in the lower part of the uterus, which can aid in the surgery.
- Healing is more efficient compared to other types of incisions.
- Sutures are more stable, reducing the risk of suture loosening.
Controlling Bleeding
During an LSCS, most bleeding originates from the angles of the incision. Specialized forceps, such as Green Armytage forceps, control bleeding.
Incision Techniques
The incision is typically made with a sharp scalpel. However, extreme care must be taken to prevent injury to the fetus, especially if the amniotic membranes are already ruptured or in emergencies such as placental abruption.
The incision may be extended on either side using scissors or through blunt dissection with the hands. When using scissors, the surgeon must ensure that a finger is placed beneath the uterus to protect the fetus from unintended injury.
Blunt dissection can help minimize intraoperative blood loss. In situations where a Pfannenstiel incision is not suitable, alternative incisions like Kronig (low vertical incision), classical (midline), or J or T-shaped incisions may be used to access the uterus.
Diagnostic And Operative Laparoscopy
Laparoscopy is a minimally invasive diagnostic procedure that utilizes a telescopic camera system to visualize abdominal and reproductive organs, including the uterus, fallopian tubes, and ovaries.
During laparoscopy, the surgeon makes tiny incisions (usually about 0.5 to 1 cm) in the abdomen through which a slender, fiber-optic tube equipped with a light and camera is inserted.
This procedure is used for diagnostic and operative purposes, allowing surgeons to biopsy suspicious growths and make repairs, ultimately avoiding more invasive open surgery.
Advantages Of Laparoscopy
Compared to open abdominal procedures, laparoscopy offers several advantages:
- Decreased blood loss
- Smaller abdominal incisions
- Reduced pain
- Shorter surgical recovery time
- Typically does not require a hospital stay
Laparoscopic Procedure and Its Uses
Laparoscopy For Diagnosis And Treatment
Laparoscopic surgery is typically performed after other infertility tests have been conducted. Patients with fertility issues, particularly those with pelvic pain indicative of endometriosis or pelvic inflammatory disease (PID), may benefit from a diagnostic and operative laparoscopy. The procedure helps identify and treat the source of pelvic pain, including issues like adhesions and scar tissue.
Examination Of Fallopian Tubes
During laparoscopy, the surgeon examines the condition of the fallopian tubes to determine if they are open. This is crucial in evaluating fertility issues.
Ectopic Pregnancy
Laparoscopy is also used to diagnose and treat ectopic pregnancies, which occur in the fallopian tube instead of the uterus, causing abdominal pain and bleeding.
Operative Laparoscopy Procedure
The procedure starts with establishing an IV line to administer fluids and relaxants. General anesthesia is then administered, ensuring you are unconscious during the procedure.
The surgeon creates a small incision in the abdomen and introduces carbon dioxide gas to expand the area, allowing for better maneuverability of the laparoscope and organ visualization.
Additional incisions are made for the laparoscope and surgical instruments. The laparoscope transmits images of your reproductive organs onto a TV screen.
The surgeon utilizes these images to examine the abdominal and pelvic organs for cysts, fibroids, adhesions, scar tissue, or endometrial growths. In some cases, a dye may be injected through the cervix to check the patency of the fallopian tubes. Tissue samples may be collected and tested for abnormalities.
Microsurgical instruments are inserted through the abdominal incisions for procedures such as cutting adhesions or removing endometriosis.
After the procedure, the incisions are closed, and you typically return home the same day. Your doctor may prescribe pain relief medication to manage any discomfort. Rest and activity restrictions are advised, especially if repairs are performed.
Common Issues Following Laparoscopic Surgery
Patients may experience several common problems after laparoscopic surgery, including
- Nausea
- Discomfort or pain around the incision sites
- A sore throat due to the breathing tube used during surgery
- Abdominal pain or tenderness
- Shoulder pain
- Abdominal bloating from the introduction of gas during the procedure
Please remember that the specific details of your laparoscopy procedure and recovery may vary, so it’s important to consult with your healthcare provider for personalized guidance and information tailored to your situation.